Introduction
Physiotherapy in Redcliffe for Upper Back Issues
Welcome to Reset My Health’s guide to Scheurmann’s Disease.
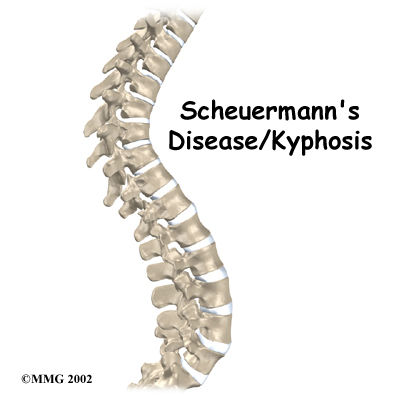
The section of spine from below the neck to the bottom of the rib cage is called the thoracic spine. From the side, the thoracic spine appears slightly rounded. Its shape is like the letter "C" with the opening of the “C” facing the front of the body. This normal curve is called a kyphosis. With an excessive kyphosis, the thoracic spine takes on a hunchbacked appearance.
Scheuermann's disease (also called Scheuermann's kyphosis) is a condition that usually starts in childhood. It affects less than one percent of the population and occurs mostly in children between the ages of 10 and 12. It affects both boys and girls with a slightly higher number of boys affected. Those who do not receive treatment for the condition during childhood often experience back pain as an adult from the spinal deformity. In some cases Scheuermann’s disease doesn’t develop until adulthood.
This guide will help you understand:
- how the problem develops
- how health care professionals diagnose the condition
- what treatment options are available
- what Reset My Health’s approach to treatment is
Anatomy
What parts of the spine are involved?
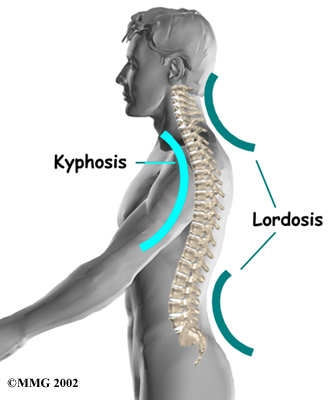
A healthy human spine has three gradual curves. From the side, the neck and low back curve gently inward. This is called a lordosis. The thoracic kyphosis (outward curve) gives the mid back its slightly rounded appearance. These normal curves help the spine absorb forces from gravity and daily activities, such as lifting.
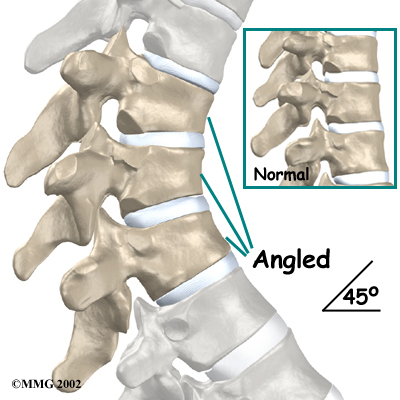
The angle of normal kyphosis in the thoracic spine varies. The angle increases slightly throughout life both in women and men. During the growth years of adolescence, a normal curve measures between 25 and 40 degrees. In general, kyphosis tends to be more exaggerated in girls. If the curve angles more than 40 degrees in either boys or girls, doctors consider the kyphosis a deformity. Scheuermann's disease causes the thoracic kyphosis to angle too far (more than 45 degrees).
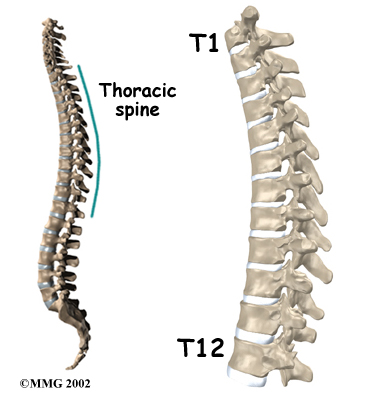
The 12 thoracic vertebrae are numbered from T1 to T12. The main section of each thoracic vertebra is a round block of bone, called the vertebral body. A ring of bone attaches to the back of the vertebral body. This ring surrounds and protects the spinal cord.
In Scheuermann's disease, the front of the vertebral body becomes wedge-shaped, possibly from abnormal growth. This produces a triangular-shaped vertebral body, with the narrow, wedged part closest to the front of the body. The wedge creates a larger bend in the kyphosis of the thoracic spine.
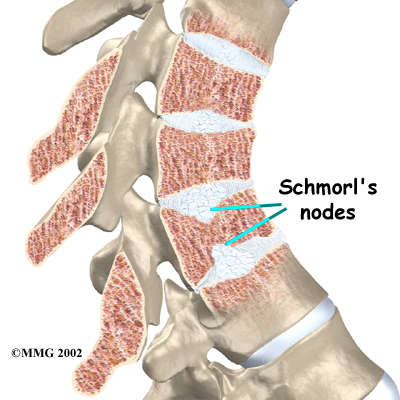
Each vertebral body is separated by an intervertebral disc, which acts like a cushion between them. There is a vertebral end plate between each disc and vertebral body. Sometimes in patients with Scheuermann's disease the material inside one or more of the discs squeezes through the vertebral end plate (which is often weaker in patients with Scheuermann's disease). This disc material forms pockets of material inside the vertebral body, a condition called Schmorl's nodes.
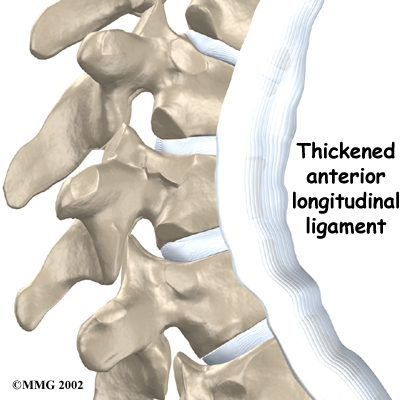
A long ligament called the anterior longitudinal ligament connects on the front of the vertebral bodies. This ligament typically thickens in patients with Scheuermann's disease and adds to the forward pull on the spine, producing more wedging and kyphosis.
Scheuermann’s disease usually produces kyphosis in the middle section of the thorax (the chest), between the shoulder blades. Sometimes, however, it can cause kyphosis in the lower part of the thoracic spine, near the bottom of the rib cage.
Related Document: Reset My Health's Guide to Thoracic Spine Anatomy
Causes
Why do I have this problem?
Famed for discovering this disease, Scheuermann himself thought a lack of blood to the cartilage around the vertebral body caused the wedging. Though scientists have since disproved this theory, the root cause of the disease is still not definitively known.
Mounting evidence suggests wedging develops as the vertebral body grows. During normal growth, the cartilage around the vertebral body develops evenly and completely into bone. If the change from cartilage to bone doesn't happen evenly, one side of the vertebral body grows at a faster rate. By the time the entire vertebral body turns to bone, one side is taller than the other. This is the wedge shape that leads to the abnormal kyphosis.
Other theories of how Scheuermann's kyphosis starts include:
- genetics
- childhood osteoporosis
- mechanical reasons
- other reasons
Genetics
Researchers have suggested that this disease can be passed down in families. Studies have shown multiple families who have passed the disease through the inheritance of certain types of genes. The genetic link is uncommon and remains under investigation.
Childhood Osteoporosis
One medical study found that some patients with Scheuermann's disease had mild osteoporosis (decreased bone mass) even though they were very young. Other studies did not show evidence of osteoporosis. More research is needed to confirm the role of osteoporosis in Scheuermann's disease.
Related Document: Reset My Health's Guide to Osteoporosis
Mechanical Reasons
Mechanical reasons include strains from bending, heavy lifting, and maintaining poor posture. This theory seems plausible because the back braces used for treating kyphosis work. If a back brace can straighten a bent spine, then perhaps mechanical forces could be causing the increased kyphosis (back braces are discussed in more detail later). Some experts think that tight hamstring muscles (along the back of the thigh) pull on the pelvis contributing to the spinal deformity.
Scientists are not convinced, however, that mechanical reasons cause the disease; rather, these factors likely aggravate the condition. In some cases, it is difficult to tell which came first: the mechanical changes causing the deformity or the deformity resulting in the anatomical and thus mechanical changes.
Other Reasons
Other theories put forth that might help explain the cause(s) of Scheuermann’s disease include biochemical changes in the collagen that make up the end-plates causing altered bone growth, above-average disc height, and increased levels of growth hormone.
Symptoms
What does the condition feel like?
A hunched posture or a round back in children usually alerts parents or teachers of the need for a visit to a health care professional. Children don't typically complain of back pain or other symptoms in the early stages of Scheuermann’s disease.
On the contrary, this is not the case in adolescents who are nearing puberty and have kyphosis in the lowest part of the thorax, near the bottom of the rib cage. In these patients, back pain is the main problem. This occurs most often in young, active males. Doctors suspect this unique form of the disease occurs because the condition is overlooked during childhood, delaying treatment.
Adults who have lived with the hunched posture for many years may note worsening pain as they age; they are disturbed by the physical changes and deformity that develop. The pain and/or the physical changes typically cause them to seek medical assistance at which time Scheuermann’s disease is discovered.
Besides having a forward curved spine, most people affected by Scheuermann's disease report back stiffness, a loss of flexibility, and some back pain. Patients generally report feeling discomfort along the sides of the spine, slightly below the main part of the abnormal curve.
The neck and low back try to compensate for the round hunched back by increasing the natural lordosis (inward curve) of these two areas. This particularly puts extra strain on the tissues of the low back. Over many years, this added wear and tear may produce low back pain, however, this mainly occurs in adults who have extra lumbar lordosis from years of untreated Scheuermann's disease.
Degenerative spondylosis is also reported as part of the natural history in middle-aged adults with Scheuermann's kyphosis. Spondylosis is when degenerative changes in the spine (usually from aging) occur. These changes can cause bone spurs to form around the spinal joints and cause the joint spaces to narrow. This can contribute to pain and stiffness in the spine.
All of these changes in spinal alignment are often accompanied by mechanical changes in other areas such as tight shoulder, hip, and leg muscles.
In rare cases of Scheuermann’s disease, the spinal cord is affected. A severe kyphosis stretches the spinal cord over the top of the curve, which can injure the spinal cord. Also, patients with Scheuermann's disease have a greater chance of having a herniated thoracic disc. With a herniated disc the material from inside the disc begins to squeeze out and press on the spinal cord. Nerve symptoms for both a stretched spinal cord as well as a herniated disc include sensations of pins and needles and numbness. In addition the leg muscles may feel weak. Symptoms from an injured spinal cord can also include changes in bowel and bladder function (particularly incontinence).
In the rare situation when the kyphosis angle exceeds 100 degrees, the sharply bent spine puts pressure on the heart, lungs, and intestines. When this occurs, patients may tire quickly, suffer shortness of breath, feel chest pain, and lose their appetite.
Diagnosis
How do health care professionals diagnose the problem?
On initial assessment at Reset My Health your physiotherapist will perform an examination that will start with a thorough history. They will ask questions about when the pain began, when and where precisely the pain occurs, your activity levels, whether you have had any previous spinal pain or problems in the past, if you have had previous treatment, what makes your pain better or worse, whether there are any noted muscle weaknesses or tingling sensations, and will ask about whether you have any problems with urination or bowel movements (particularly incontinence). They will also want to know if you have pain in any other areas of your body such as your hips, knees, or shoulders. They may also ask questions about your sport, school, or work activities.
A physical examination will be done once the history is complete.
Your physiotherapist will examine your thoracic spine along with the other areas of the back to evaluate the curves of the spine, spasm of the muscles, unusual markings on the skin or soft tissues along the spine and will assess your overall posture and alignment of the back as well as your lower extremities. Your physiotherapist will palpate, or touch along the spine and over the muscles to determine if any particular areas are painful or tight. They may push on the spine, or manually move the spine to get a general idea of how much motion is available at each segment.
Your physiotherapist will also examine your hips, knees, and ankles to determine if these joints and the muscles that are involved with them might be contributing to the pain you feel in your back. The length (flexibility) and strength of the muscles of the buttocks, the front of the hip, as well as the thigh (quadriceps and hamstrings muscles) are particularly important areas that your physiotherapist will assess. These muscles can create an abnormal pull on the back if they are too tight, or not support the back well enough if they are too weak. Both tightness and/or weakness can contribute to your back pain. The hip joints themselves, if restricted in their ability to move through a full range of motion, can particularly contribute to back pain so their motion will be thoroughly assessed.
Your physiotherapist will also want to examine your ability to bend your back forwards, backwards, sideways, as well as rotate it and to get into positions involving a combination of these motions. Assessing this movement in the thoracic spine may include having you raise your arms up overhead or put them behind your neck.
Your physiotherapist will also look at your posture and alignment while you are standing and sitting, and may also want to watch you during different activities such as walking, squatting, jumping, lifting one leg, or kneeling on your hands and knees. As your physiotherapist observes you performing these activities they will determine the ability for you to support your trunk with the deep muscles of the abdominal area and back.
A neurological examination may need to be done which will include checking your reflexes, sensation, and muscle strength.
After a thorough history and physical examination Scheuermann’s disease may be suspected. The only way to definitely diagnose Scheuermann's kyphosis, however, is with an X-ray.

Investigations
Taken from the side, an X-ray may show vertebral wedging, Schmorl's nodes, and changes in the vertebral end plates. Doctors use X-ray images to measure the angle of kyphosis. An official diagnose of Scheuermann's disease is made when three vertebrae in a row wedge five degrees or more and when the kyphosis angle is greater than 45 degrees.
A side-view X-ray can also show if the spine is flexible or rigid. Patients are asked to bend backwards and hold the position while an X-ray is taken. The spine straightens easily when it is flexible. In patients with Scheuermann's disease, however, the curve stays rigid and does not improve by trying to straighten up.
From the front, X-rays show if the spine curves from side to side. This sideways curve is called a scoliosis and occurs in about one-third of patients with Scheuermann's kyphosis.
X-rays can also show signs of wear and tear in adults (spondylolysis) who have extra lumbar lordosis from years of untreated Scheuermann's disease.
A Computed Tomography scan (CT) may be ordered. This is a detailed X-ray that lets doctors see slices of the body's tissue.
Myelography is a special kind of X-ray test. For this test, dye is injected into the space around the spinal canal. The dye shows up on an X-ray. This test is especially helpful if the doctor is concerned whether the spinal cord is being affected.
Magnetic resonance imaging (MRI) may be ordered. An MRI uses magnetic waves rather than X-rays to show the soft tissues of the body. This machine creates pictures that look like slices of the area being examined. This test does not require special dye or a needle.
Scheuermann's disease or kyphosis, once definitively diagnosed, is determined as either being typical (Type I) or atypical (Type II). These two forms of the disease affect different parts of the spine. The typical form (most common type) has the thoracic kyphotic pattern described in this section. In these cases the lower (lumbar) spine compensates by developing an increased lordosis curve. This curve is termed ‘hyperlordotic’, which means the curve has increased beyond what is considered “normal.”
The atypical form of Scheuermann’s disease (Type II) affects the low back known as the lumbar spine. It is the upper part of the lumbar spine (where the thoracic spine transitions to become the lumbar spine) that is involved. Type II is seen most often in young boys before puberty who are active in sports activities. They experience pain that goes away with rest and changes in position or activity level.
Reset My Health provides services for physiotherapy in Redcliffe.
Treatment
What treatment options are available?
Nonsurgical Treatment
A child or youth with a mild kyphosis may simply need to be observed for changes in the curve, as well as be educated on their posture and activities from a physiotherapist.
Unless the curve or pain becomes worse, no other treatment may be needed. Some children eventually improve without having a noticeable abnormal kyphosis and have no long-term problems. Others may always have a mildly exaggerated thoracic kyphosis but are able to function normally without subsequent pain or other problems.
If your doctor is concerned that the curve will worsen, he or she may suggest bracing along with exercise. A brace is most effective when used before the skeleton matures at about age 14. Doctors commonly chose a Milwaukee brace, which is made of molded plastic that conforms to the waist and is designed to hold the shoulders back and gradually straighten the thoracic curve. On the back, two upright, padded bars line up along the sides of the spine. Pressure from the upright bars straightens the spine. The brace won't reverse the curve in a fully developed spine, nor is it helpful for rigid curves that angle more than 75 degrees.
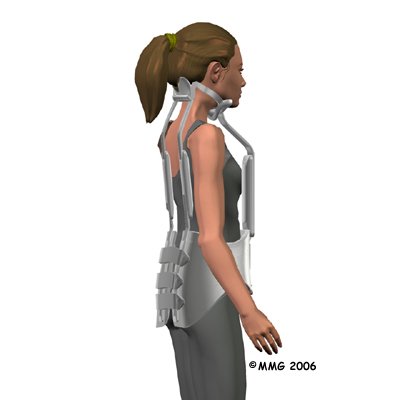
Younger patients (under 15) generally wear the brace all the time including at night, although they usually remove the brace to shower. The doctor adjusts the brace regularly as the curve improves. When the thoracic curve has improved enough, the brace is worn part-time (eight to 12 hours per day) until the skeleton is done growing, which is typically around age 14 or 15.
Sometimes adults obtain partial correction of the kyphosis and pain relief with bracing even though they have reached full bone growth. Bracing for pain relief in adults is also considered when surgery is not an option.
Physiotherapy is recommended in combination with bracing. Exercises appear to maximize the effect of the brace by strengthening muscles that help align the spine. In addition, advice from a physiotherapist regarding posturing and activity modification can be extremely useful in the treatment of Scheuermann’s kyphosis. Even if a brace is not used, physiotherapy at Reset My Health is recommended to assist with any pain that may be present, to teach proper posturing for the spine, and to assess and treat any muscular imbalances that may be affecting the mechanical pull on the spine.
Doctors may prescribe anti-inflammatory medication for pain. Younger patients generally use this medicine on a short-term basis, in combination with other treatments. Adults who have ongoing pain sometimes require long-term use of anti-inflammatory medication.
Surgery
Surgeons rarely recommend fusion surgery for Scheuermann's disease, however certain situations may require it. For example, surgery may be needed if the pain becomes severe and doesn't go away with nonoperative treatment or if pressure on the spinal cord or spinal nerves is causing problems. Patients with a rigid kyphosis that angles more than 75 degrees may also need surgery. In these cases the entire length of the kyphosis is fused to prevent further deformity. In other cases people request surgery if the deformity is severe enough that their appearance causes them considerable psychological and/or emotional distress.
Two procedures commonly used to treat thoracic kyphosis are:
- posterior fusion
- combined fusion
Posterior Fusion
In a fusion operation, two or more bones are joined into one solid bone. Surgeons perform posterior fusions for Scheuermann's disease on the rare patient who prefers not to use a brace and whose spine is still growing, is mildly flexible, and has a kyphosis of less than 65 degrees.
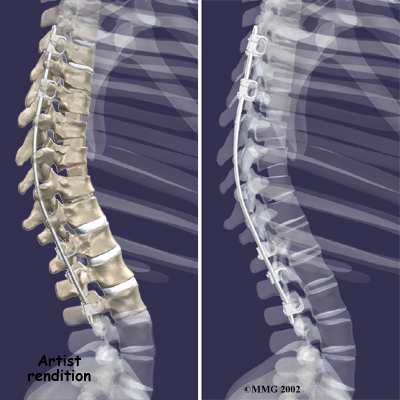
This surgery is done through the back (posterior) portion of the spine, as opposed to an anterior approach, which is done from the front. After making an incision in the back, the surgeon applies pressure to straighten the kyphosis. Small strips of bone graft are then laid over the back of the spinal column. These strips encourage the bones to grow together. Metal rods are attached along the spine to prevent the vertebrae from moving. The rods hold the spine in better alignment and protect the bone graft so it can heal better and faster.
A posterior approach has the advantage of less blood loss than an anterior approach and does not interfere with major anterior blood supply to the spinal cord. Surgical time is also shorter with the posterior method. Improved instrumentation and surgical technique has improved results for posterior fusions. Many more surgeons are using this approach with fewer problems even with more rigid curves.
Combined Fusion
Combined fusion is actually two fusion surgeries, one from the back of the spine (posterior) and one from the front (anterior.) In the past, two separate operations were needed, but now some surgeons do both fusions in the same operation. This surgery is commonly used if the spine is finished growing and the kyphosis angle is more than 75 degrees.
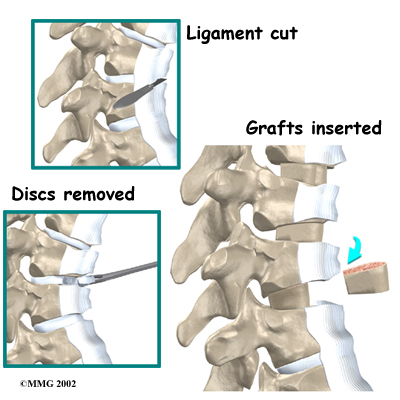
The surgeon starts with an anterior fusion. With the patient on his or her side, the surgeon cuts away a piece of rib to make a small opening on the side of the thorax. The rib opening is spread apart so the surgeon can reach the spine better. The surgeon operates on the front of the spine through the chest cavity.
Next a section of the anterior longitudinal ligament is cut. This makes it easier to straighten the hunched spine. The intervertebral discs in the problem area are taken out, and the spaces between the wedged vertebrae are filled with bone graft. One method is to take a graft of bone from the pelvis and tamp it into the place of each removed disc. This requires another incision over one side of the pelvis. A second method is to grind up the piece of rib that was removed and place it in the disc spaces.
As the grafts heal, the vertebrae become fused into solid bone.
The second part of the surgery is a more involved form of a posterior fusion using special rods and hooks. This part of the operation can be done right after the anterior fusion or scheduled for one week later.
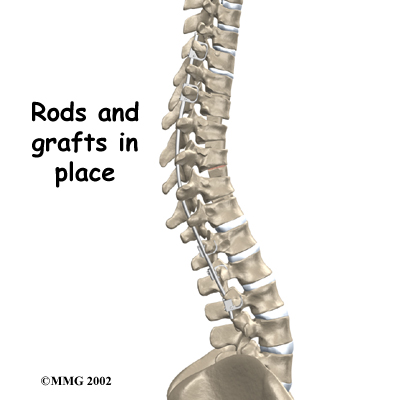
For this part of the combined fusion surgery the surgeon makes an incision over the back of the spine. The skin and muscles are spread apart then strips of bone graft are laid across each vertebra to be fused. Long rods are inserted along the sides of the spine. The rods have hooks attached on both ends. Wire is wrapped between the top and bottom hooks. Tightening the wires causes the spine to straighten. The rods help hold the spine steady as the bone grafts heal. The rods are usually left in permanently.
Final results are overall favorable following surgery for Scheuermann’s disease. The majority of patients report being satisfied with their cosmetic appearance. Some patients even experience complete relief from their pain. There may be some low back pain or discomfort with strenuous activity.
Complications following surgery are rare but can include infection, loss of correction, spinal cord injury or other neurologic problems. In a small number of cases, a second surgical procedure may be required.
Post Surgical Rehabilitation
The amount of time spent in the hospital after surgery for Scheuermann’s disease depends on exactly what was done in surgery. Although some patients leave the hospital shortly after surgery, some surgeries require patients to stay in the hospital for a few days. If your surgeon recommends it a physiotherapist may visit while you are in the hospital to assist as you start moving and to give advice on how to move and do everyday activities without putting extra strain on the back. Gentle back range of motion or isometric (tightening muscles without moving the body or joints) core stability exercises may be initiated if the surgeon allows it but any specific movement restrictions implicated by the surgeon will be strictly abided by. Generally patients should be cautious about overdoing any activities in the first few weeks after surgery in order to allow the fusion to heal.
During recovery from surgery, patients may need to wear a back brace or support belt. Your surgeon will determine how long the brace is required.
Physiotherapy at Reset My Health may begin as soon as the surgeon recommends it. Generally patients wait up to three months before beginning a rehabilitation program after fusion surgery for Scheuermann's disease. This allows the fusion itself to heal before subjecting it to any stress. Once you begin you will typically need to attend therapy sessions for eight to 12 weeks. In some cases this time frame may be longer, depending on how you are recovering. Full recovery may take up to eight months, and regular treatment sessions at Reset My Health will decrease over time, although you will still be required to regularly do your home exercise program.
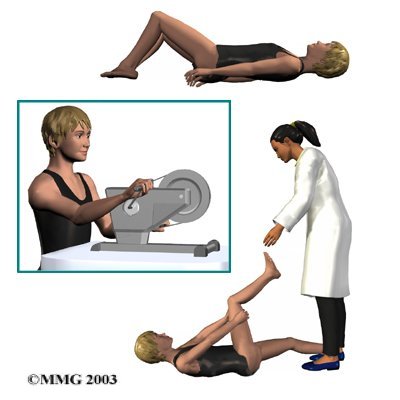
During the first few appointments at Reset My Health following surgery for Scheuermann’s disease treatment will focus on relieving any residual pain that may be lingering from the surgery. Your physiotherapist may use modalities such as heat or ice to assist with decreasing any pain or swelling. In some cases ultrasound, or electrical current may be used. Your physiotherapistmay also use hands-on techniques such as massage or mobilizations to improve motion and relieve discomfort.
Your physiotherapist will immediately begin with range of motion exercises for your back. Your hips also need to be able to move through their full range of motion in order for your back to not take added stress, so range of motion exercises for your hips will also be prescribed. If overall movement is particularly difficult or continues to be restricted by pain, your physiotherapist may suggest that you do your therapy exercises in a physiotherapy pool where the warmth of the water and the hydrostatic properties can assist with decreasing pain and make motion easier. Your physiotherapist will discuss this with you if they feel it is appropriate.
Core strengthening after spinal surgery is particularly important so exercises targeting this will begin as soon as possible. Your physiotherapist will teach you how to use your core muscles, and will prescribe specific exercises for you to improve your core control, strength and endurance. They will also encourage you to use the core muscles during everyday activities such as sitting, walking, or getting out of bed. As you progress in your rehabilitation you will also be asked to incorporate core strengthening into more advanced activities such as during any physical exercise. While learning to activate these muscles, your physiotherapist may use taping techniques to help provide feedback or, if needed, to provide ongoing support for your back as you move towards doing your normal activities.
Other stretches and strengthening exercises that target your individual muscular imbalances will also be incorporated into your rehabilitation program. These exercises will address any tight, weak, or overactive muscles identified that may restrict your back from moving optimally or may contribute to back pain in the future. General strengthening exercises for your buttocks muscles will be prescribed in all cases as these muscles are crucial in supporting the low back area, which subsequently supports the thoracic spine. Strength exercises for those muscles of the back that extend the spine and assist in maintaining posture will also be added.
As mentioned above, the ability for the lungs to expand normally can be compromised with Scheuermann’s kyphosis. Your therapist may prescribe aerobic type exercises after surgery to maintain or improve lung function and to assist with maintaining the space available for the lungs within the cavity of the thorax.
As an important component of your treatment your therapist will discuss proper posture and alignment with you. Proper posture is crucial during all exercises as well as during everyday activities. If necessary your therapist will discuss ways to modify your regular activities or move differently to accommodate your fused spine. Maintaining good posturing as often as possible can help to prevent back pain in the future or can at least decrease the incidence or severity of back pain that may arise.
Slowly your therapist will assist you with returning to your normal activities. If your surgeon has indicated any permanent activity restrictions then your therapist will discuss these with you. Generally rehabilitation after surgery for Scheuermann’s disease progresses very well with the treatment we provide at Reset My Health. If, however, your pain continues longer than it should or therapy is not progressing as your physiotherapist would expect, we will ask you to follow-up with your surgeon to ensure your back is tolerating the rehabilitation well and to ensure there are no hardware issues that may be impeding recovery.
Portions of this document copyright MMG, LLC.
Reset My Health provides services for physiotherapy in Redcliffe.
 Get Immediate Access To Your Special Report And Top Tips From Our PTs!
Get Immediate Access To Your Special Report And Top Tips From Our PTs!


