Introduction
Physiotherapy in Redcliffe for Cervical Spinal Stenosis
Welcome to My Health Team's resource for Cervical Spinal Stenosis.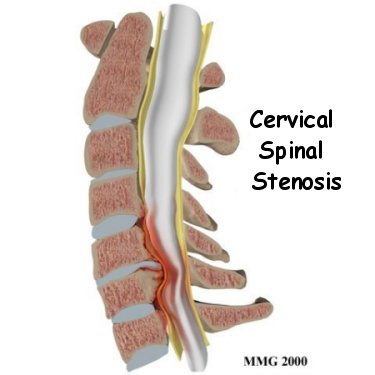 The spinal cord is a column of nerve tissue protected by a bony tube in the spinal column. Conditions that narrow the space in this tube put the spinal cord at risk of getting squeezed. This narrowing is called stenosis. When the narrowing occurs in the spinal column of the neck it is called cervical spinal stenosis, or cervical stenosis. Pressure against the spinal cord as a result of spinal stenosis causes injury to the spinal cord, which is termed myelopathy. Myelopathy is a condition that demands medical attention as it can cause serious problems including problems with the bowels and bladder, changes in the way you walk, and can affect your ability to use your fingers and hands.
The spinal cord is a column of nerve tissue protected by a bony tube in the spinal column. Conditions that narrow the space in this tube put the spinal cord at risk of getting squeezed. This narrowing is called stenosis. When the narrowing occurs in the spinal column of the neck it is called cervical spinal stenosis, or cervical stenosis. Pressure against the spinal cord as a result of spinal stenosis causes injury to the spinal cord, which is termed myelopathy. Myelopathy is a condition that demands medical attention as it can cause serious problems including problems with the bowels and bladder, changes in the way you walk, and can affect your ability to use your fingers and hands.
This guide will help you understand:
- the anatomy of the spine and neck
- what causes cervical spinal stenosis
- how the condition is diagnosed
- what treatment options are available
- what My Health Team’s approach to rehabilitation is
Anatomy
What parts make up the spine and neck?
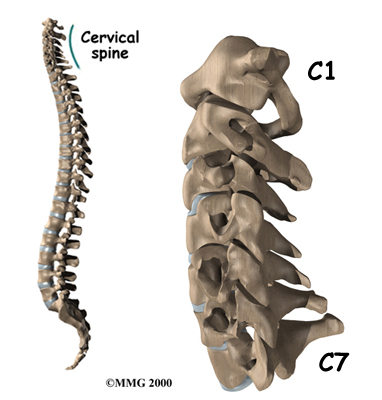
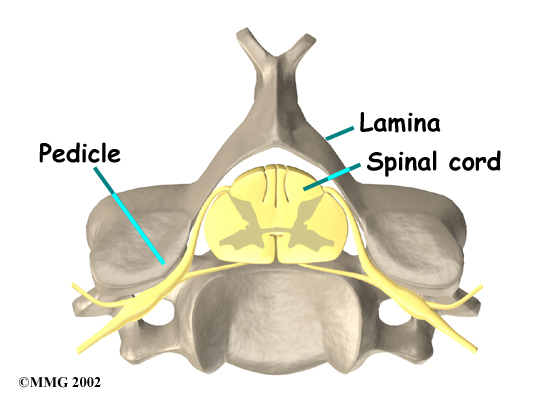
The spine is made up of a column of bones called vertebrae. A round block of bone, called a vertebral body, forms the bulk of each vertebra. A bony ring attaches to the back of the vertebral body, forming a canal. Two parts form this bony ring. The first part, the pedicle, attaches to the back of each vertebral body. Each pedicle bone connects with the second part of the ring, called the lamina. The two laminas meet at the back and form into the part of the vertebrae called the spinous process, which is the pointy part you can feel at the back of your neck. The lamina forms a protective roof over the back of the spinal cord. When the vertebra bones are stacked on top of each other, the bony rings of the vertebrae form a long bony tube that surrounds and protects the spinal cord as it passes through the spine.
An intervertebral disc fits between each vertebral body and provides a space between the spine bones. The disc works like a shock absorber and protects the spine against the daily pull of gravity. The disc also protects the spine during activities that put strong force on the spine, such as jumping, running, and lifting.
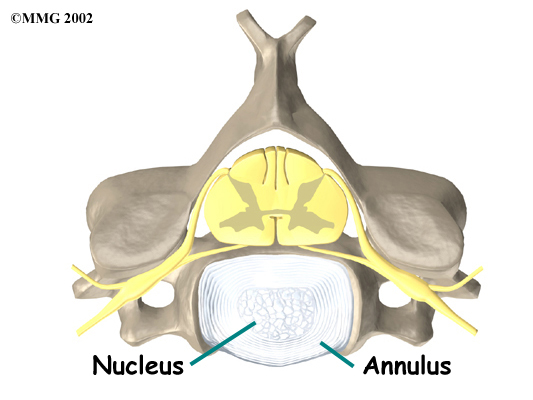
An intervertebral disc is made up of two parts. The center, called the nucleus, is spongy. It provides most of the ability to absorb shock. The nucleus is held in place by the annulus, a series of strong ligament rings surrounding it.
These ligaments also help to resist rotation and shearing in the spine. Ligaments are strong connective tissues that attach bones to other bones.
Related Document: My Health Team's Guide to Cervical Spine Anatomy
Causes
Why do I have this problem?
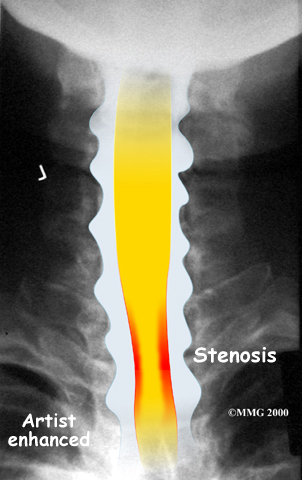
The bony spinal canal normally has more than enough room for the spinal cord. Typically, the canal is just less than ¾ of an inch, or 17-18 millimeters around, which is less than the size of a small bottle cap. Spinal stenosis occurs when the canal narrows to around half an inch, or 13 millimeters or less. When the size drops even further, severe symptoms of myelopathy occur. The symptoms of myelopathy result from the actual pressure against the spinal cord itself as well as the reduced blood supply in the spinal cord as a result of the pressure.
Spinal stenosis may develop for any number of reasons. Some of the more common causes of spinal stenosis include:
- degeneration
- congenital stenosis
- spinal instability
- disc herniation
- constriction of the blood supply to the spinal cord
- chronically poor posture
Degeneration
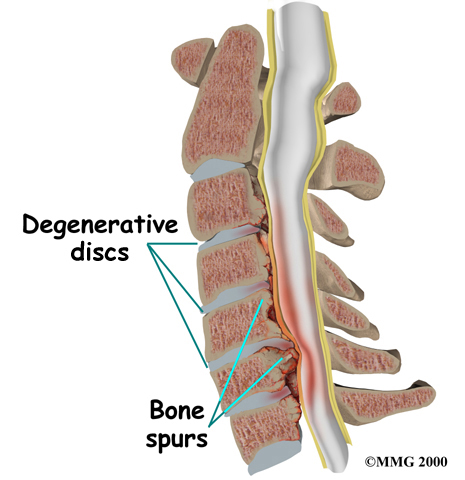
Degeneration is the most common cause of spinal stenosis. Wear and tear on the spine from normal aging and from repeated stress and strain can cause many problems in the cervical spine. The intervertebral disc can begin to collapse, shrinking the space between the vertebrae. Bone spurs (small bony projections) may form that protrude into the spinal canal and reduce the space available for the spinal cord. The ligaments that hold the vertebrae together may become thicker and can also push into the spinal canal. All of these conditions narrow the spinal canal.
Congenital Stenosis
Some people are born with a spinal canal that is narrower than normal. This is called congenital stenosis. They may not feel problems early in life, but having a narrow canal to begin with places them at risk for stenosis. Even a minor neck injury can set people with a smaller spinal canal up to have pressure against the spinal cord. People who are born with a narrow spinal canal often have problems later in life, because the already narrowed canal tends to become even narrower due to the normal degenerative effects of aging.
Spinal Instability
Spinal instability can cause spinal stenosis. Spinal instability means that there is extra movement among the bones of the spine. Instability in the cervical spine can occur if the supporting ligaments have been stretched or torn from a severe injury to the head or neck. Alternatively spinal stability can occur in people who have diseases that loosen their connective tissues. For example, rheumatoid arthritis can cause the ligaments in the upper bones of the neck to loosen, allowing the topmost neck bones to shift and close off the spinal canal. Whatever the cause, extra movement in the bones of the spine can lead to spinal stenosis and myelopathy.
Disc Herniation
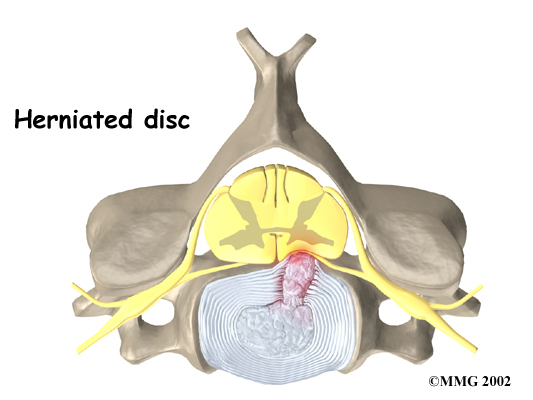
Spinal stenosis can occur when a disc in the neck herniates. Normally, the shock-absorbing disc is able to handle the downward pressure of gravity and the strain from daily activities. However, if the pressure on the disc from everyday activities becomes too much or there is an injury which damages the disc, such as a blow to the head or neck, the nucleus inside the disc may rupture through the outer annulus and squeeze out of the disc. This is called a disc herniation. If an intervertebral disc herniates straight backwards, it can press against the spinal cord and cause symptoms of spinal stenosis. If it herniates to the side instead of straight back it generally compresses the smaller nerves which leave the spinal column rather than the spinal cord itself.
Constriction of the blood supply to the spinal cord
The changes that happen with degeneration and disc herniation can choke off the blood supply to the spinal cord. The sections of the spinal cord that don't get blood have less oxygen and don't function normally, which leads to symptoms of myelopathy.
Symptoms
What does cervical stenosis feel like?
Cervical stenosis usually develops slowly over a long period of time. This is partly because degeneration in later life is the main cause of spinal stenosis. Symptoms rarely appear all at once when degeneration is causing the problems. A severe injury or a herniated disc may cause symptoms to come on immediately.
Most patients with cervical spinal stenosis have problems with their hands. The area where the spinal cord is compressed in patients with cervical stenosis is very close to the nerves that go to the arm and hand. The problem that compresses the spinal cord in the neck may also compress the nerves where they leave the spinal column. The main complaint is that their hands start to feel numb. The pressure can also cause numbness on the skin of the arm or hand. Due to the weakness in the muscles that develops from the pressure on the nerves supplying the muscles, another complaint is that the patient feels clumsy when doing fine motor activities like writing or typing. Gripping and letting go of items also becomes difficult because the muscles along the inside edge of the palm and fingers weaken. Nerve pressure can also cause pain, which can radiate from the neck to the shoulder, upper back, or even down one or both arms.
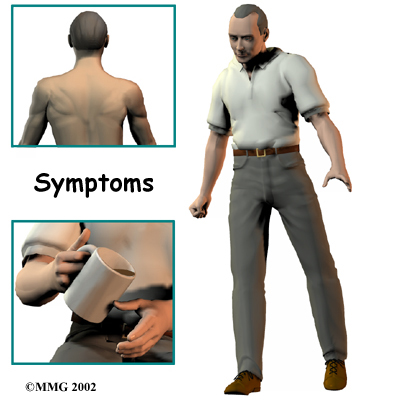
Shoulder weakness is a symptom that also develops in many patients. This happens most often when the spinal cord is compressed in the upper part of the neck. The deltoid muscle, which covers the top and outside of the shoulder, and the shoulder blade muscles are the most affected muscles. These muscles weaken and begin to show signs of wasting (atrophy) from not receiving adequate nerve input.
In some patients the first sign of cervical spinal stenosis to appear is a change in the way they walk. Patients don't realize this problem is coming from their neck but the pressure on the spinal cord in the neck can not only affect the arms, but can also affect the nerves and muscles in the legs, which leads to changes in the way they walk. Eventually their walking pattern gets jerky and they lose muscle power in their legs.
Pressure against the spinal cord can also create problems with the bowels and bladder. Mild spinal cord pressure makes you feel like you have to urinate more often but it also makes it difficult to get urine to flow (urinary hesitancy). Moderate disturbances cause people to have a weak flow of urine, which makes them dribble urine. In addition they also have to strain during bowel movements. In severe cases, people aren't able to voluntarily control their bladder or bowels; this is called incontinence.
Diagnosis
How will my healthcare professional identify the condition?
Diagnosis begins with a complete history and physical examination. Your healthcare professional will inquire about what your symptoms are, such as pain, tingling or numbness, clumsiness, weakness in your hands or legs, and difficulties walking. They will want to know where exactly your symptoms are, when your symptoms started, and if your symptoms are getting better or worse. They will also want to know if your symptoms came on gradually or if you feel that they were associated with a specific traumatic event. Your healthcare professional will also inquire about how your problem is affecting your daily activities such as work, home duties, or any recreational activities you may be involved in.
Next your healthcare professional will do a physical examination. They will assess your neck range of motion by either asking you to put your neck into a variety of positions or placing your neck into specific positions in order to see which neck movements cause pain or other symptoms. They will want to feel your neck and check the mobility in the joints. Next they will want to check the strength in your arms, hands, and legs and may also assess the range of motion of these joints. Your skin sensation and reflexes will also be tested. Your healthcare professional will also want to watch you walk to see if there are any subtle changes in your walking pattern.
Investigations
What investigations may need to be done?
X-rays are used to look for the cause of pressure against the spinal cord. X-ray images can show if degeneration has caused the space between the vertebrae to collapse and may show if a bone spur is pressing against the spinal cord.
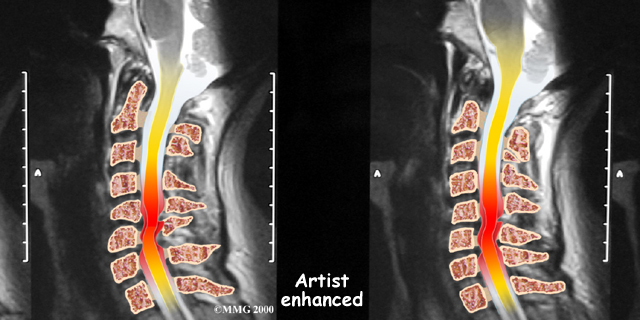
If more information is needed, a magnetic resonance imaging (MRI) scan may be ordered. The MRI machine uses magnetic waves rather than X-rays to show the soft tissues of the body. This test gives a clear picture of the spinal cord and can show where it is being squeezed. An MRI machine creates pictures that look like slices of the area your healthcare professional is interested in. This test does not require any special dye or a needle.
A computed tomography (CT) scan may also be ordered. The CT scan is a detailed X-ray that lets doctors see slices of bone tissue. The image can show if bone spurs are protruding into the spinal column and taking up space around the spinal cord.
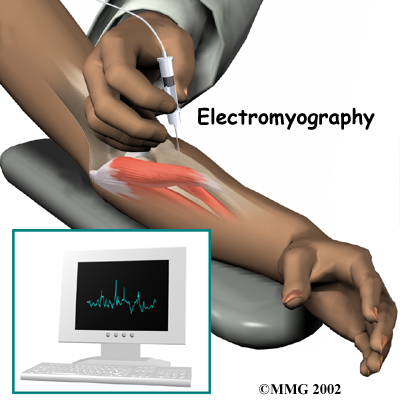
In addition to any of the above tests it may also be recommended that you have electrical tests of the nerves that go to your arm and hand. An electromyography (EMG) test is used to check if the motor pathway in a nerve is working correctly. A somatosensory evoked potential (SSEP) test may also be requested in order to locate more precisely where the spinal cord is getting squeezed. The SSEP is used to measure whether a nerve is able to receive and send sensory information such as pain, temperature, and touch. The function of a nerve may be recorded with an electrode placed over the skin or with a needle that is inserted into the nerve or sensory center of the brain.
Treatment
What can be done for cervical spinal stenosis?
Nonsurgical Treatment
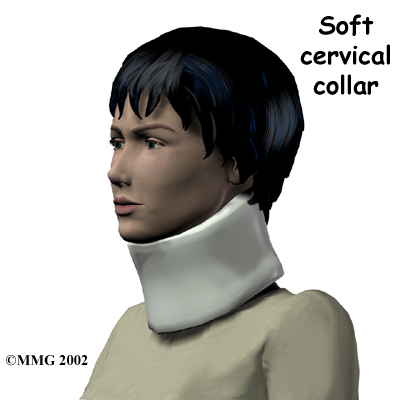
In acute situations, at first your healthcare professional may suggest immobilizing the neck with a soft neck collar. The collar is a padded ring that wraps around the neck and is held in place by a Velcro strap. Keeping the neck still for a short time can calm inflammation and pain. Patients wear the collar during waking hours for up to three months, and only take it off to shower and engage in rehabilitation. Slowly the time that the collar is worn each day is tapered.
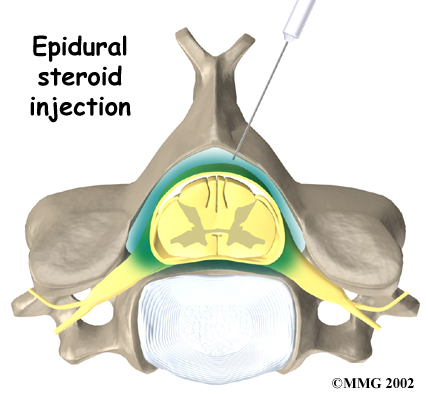
Some patients are given an epidural steroid injection (ESI). The injection is given in a part of the spinal canal called the epidural space. This is the area between the dura (the material that covers the spinal cord) and the spinal column. It is thought that injecting steroid medication into this space fights inflammation around the nerves and discs. This can reduce the swelling and give the spinal cord more room.
Non-surgical Rehabilitation
Physiotherapy at My Health Team can be very useful for cervical spinal stenosis if the disease has not progressed too far. Our treatment will focus on relieving your pain and improving your range of motion. Depending on what your exact symptoms are, your rehabilitation will also focus on maintaining or improving the strength and coordination in your hands and legs, as well as potentially assist in decreasing any altered sensations of your skin that you may be feeling.
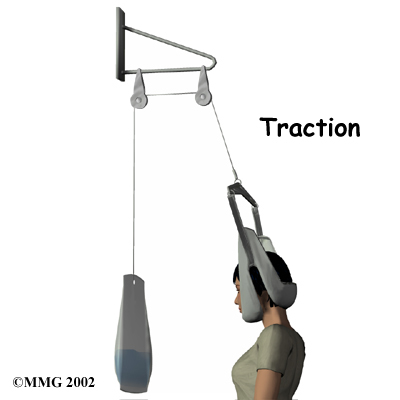
Your therapist may use a variety of modalities to assist with your symptoms. Many patients find heat applied to the neck is comforting. Ice may also be used, if preferred. In addition, electrical modalities such as ultrasound or interferential current may also be used. Hands-on treatment such as massage, stretches or traction of the neck can also be very useful. Traction is a way to gently stretch the joints and muscles of the neck. It can be done using a machine with a special head halter, or your therapist can apply the traction with their hands. They can also teach you how to perform self-traction while at home, which may also assist with your symptoms.
Your therapist will prescribe a series of range of motion exercises for your neck, and also for related areas such as your shoulders. These exercises may be done under the supervision of your therapist in the clinic but will also be required to be done as part of your home exercise program. Strengthening exercises are also an extremely important part of your rehabilitation if you suffer from cervical spinal stenosis. As explained above, the muscles supplied by nerves that are being affected by the stenosis will become weak. By doing strengthening exercises the muscles have a better chance at maintaining the strength they already have or improving any strength which has been lost.
Coordination exercises may be prescribed in addition to the strength exercises in order to get the muscles of the hands (and feet, if necessary) working well. Proprioception exercises, which assist with the ability to know where your body is in space, will be also be prescribed.
If you have lost any sensation due to your cervical spinal stenosis then your therapist may also prescribe exercises to help maintain or improve your sensation. Even simple hand-rubbing can help to stimulate your sensation if it has been altered.
If necessary, your therapist will encourage gait-retraining exercises. If you are not walking normally due to the effects of the spinal stenosis, your gait will not be as efficient as it should be, and this abnormal pattern can lead to secondary injuries. If necessary, your therapist will prescribe a walking aid such as a cane or stick in order to ensure you are safe and prevent any falls while you are improving your walking pattern.
Maintaining good posture is very important when dealing with cervical spinal stenosis. Your therapist will ensure that you know what the proper posturing position is for when you are sitting, standing, walking or engaging in any other regular activity you do. Due to the already small anatomical area in the neck for the nerves and spinal cord to be contained, poor posturing can make a significant difference to the symptoms you feel. In order to assist your posturing or aid your symptoms, your therapist may use tape near your neck or shoulder areas or in some cases may even suggest the use of a specialized brace that assists with maintaining posture.
Lastly, your therapist will educate you on the importance of restricting any aggravating activities that you engage in during the day. Heavy and repeated motions of the neck, arms, and upper body can be particularly irritating to cervical spinal stenosis. Your therapist can also provide advice on the best sleeping posture to aid your symptoms.
Unfortunately spinal myelopathy caused by cervical spinal stenosis can be a very serious condition. If your condition is causing significant problems or is rapidly getting worse, immediate surgery may be recommended rather than trialling any non-surgical treatments.
My Health Team provides services for physiotherapy in Redcliffe.
Surgery
What surgical procedures may be done?
When there are signs that pressure is building on the spinal cord, surgery may be required, and sometimes it is required immediately. Surgeries used to treat spinal stenosis include:
- Laminectomy
- Discectomy and fusion
- Corpectomy and strut graft
- Laminectomy
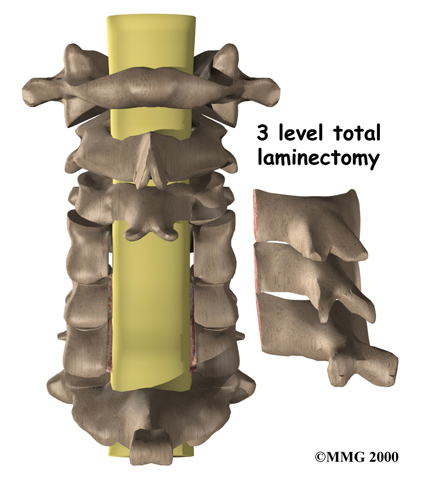
As explained under ‘Anatomy’, the lamina is the bony covering layer of the spinal canal. It forms a roof-like structure over the back of the spinal cord. When bone spurs or disc contents have pushed into the spinal canal, a laminectomy is done to take off the lamina bone in order to release pressure on the spinal cord.
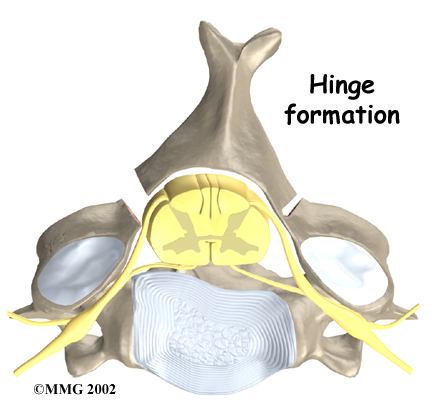
Some surgeons completely remove the entire lamina bone, which is called a total laminectomy. Others prefer to keep the lamina in place by forming a hinge on one edge of the bone. Cutting partially through the lamina on one side forms this hinge. A second cut is made all the way through the lamina on the other side, which is then lifted away from the spinal cord. The hinged side eventually forms a bone union, which holds the opposite side open and keeps pressure off the spinal cord.
Related Document: My Health Team's Guide to Cervical Laminectomy
Anterior Cervical Discectomy and Fusion
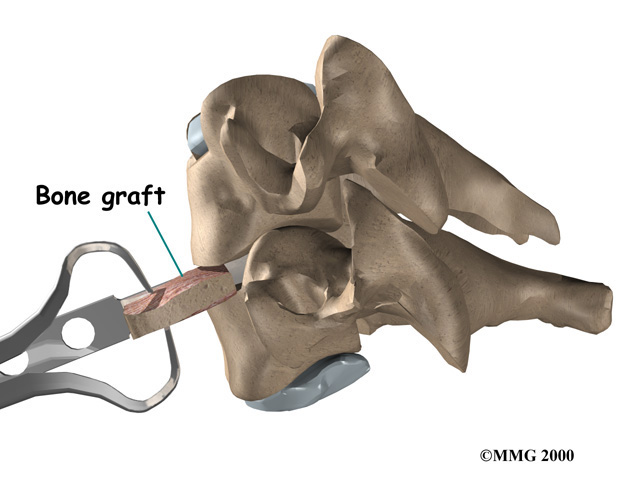
A fusion surgery joins two or more bones into one solid bone. Fusion of the neck bones is most often done through the front of the neck. During this surgery the surgeon takes out the intervertebral disc (discectomy) between two vertebrae. A layer of bone is shaved off the flat surfaces of the two vertebrae to be fused. This causes the surfaces to bleed which in turn stimulates the bone to heal. (This is similar to the way two sides of a fractured bone begin to heal.) A section of bone is grafted from the top part of the pelvis bone and inserted into the space where the disc was taken out. This separates the two vertebra bones, taking pressure off the spinal cord. As the bone graft heals in place, the vertebral bones fuse together into one solid bone.
Related Document: My Health Team's Guide to Anterior Cervical Discectomy and Fusion
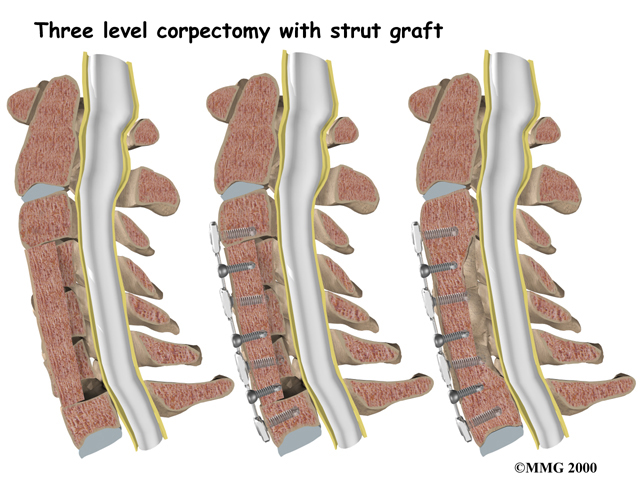
Corpectomy and Strut Graft
A corpectomy relieves pressure over a large part of the spinal cord. In this procedure, the surgeon takes off the front part of the spinal column and removes several vertebral bodies. The spaces are then filled with bone graft material. Metal plates and screws are generally used to hold the spine in place while it heals. A corpectomy is used in cases of severe spinal stenosis.
Related Document: My Health Team's Guide to Cervical Corpectomy and Strut Graft
Post-surgical Rehabilitation
What should I expect after surgery?
Your post-surgical rehabilitation will depend on which surgical procedure you have had done. Some patients leave the hospital shortly after surgery, but some surgeries require patients to stay in the hospital for a few days. A physiotherapist may see you to initiate treatment in your hospital room after surgery. These initial therapy sessions are designed to help you learn how to move about and begin doing routine activities without putting extra strain on your neck. Your therapist will remind you of using proper posturing during all your activities and will give you tips on comfortable and safe sleeping habits. Depending on the surgery you have had done and the post-surgical rehabilitation protocol of your specific surgeon, range of motion and gentle strengthening exercises may be started.
In cases where a fusion or graft has been done, you may be placed in a halo vest or rigid neck brace. These braces are used to restrict the motion in the neck in order to allow the fusion to heal. Bone fusion may take several months. When the surgeon is absolutely certain the bones have fused together, you will be able to discontinue using the neck brace or halo vest.
Once your surgeon recommends it, you can begin post-surgical rehabilitation at My Health Team. During your first few appointments at My Health Team your physiotherapist will focus on relieving any pain and inflammation that may exist from the surgical procedure itself. We may use modalities such as ice, heat, ultrasound, or electrical current to assist with decreasing any pain or swelling you have around the surgical site or any related areas.
Due to the effects of your surgery as well as any period of immobilization in a brace, your neck range of motion will be restricted. Your therapist will prescribe range of motion exercises for you to do at the clinic and to also do as part of your home exercise program. It should be noted that you may lose a small portion of your overall range of motion due to the surgical procedure you have had done, but your therapist will ensure that you maximize your available range of motion, and that you are moving well within whatever range of motion you have.
If you have been wearing a neck brace for any period of time then your neck muscles will be weak and deconditioned. Even if you have not been in a brace, the neck muscles can be weak and deconditioned due to the pain and original symptoms of the cervical stenosis. Any area that has become weak will require strengthening. Your therapist will also prescribe strengthening exercises for your neck as well as related areas such as your shoulders, upper back, and core area. Your therapist will focus on ensuring that you perform all your exercises with precise technique in order to avoid any secondary injuries. Maintaining good posture during all of your activities of daily living will also help to strengthen your muscles. For this reason your therapist will be adamant in reminding you of proper posturing technique and will encourage it as often as possible. You will need to be extremely cautious about overdoing activities in the first few weeks to months after surgery. Your therapist will be crucial in guiding you in regards to your exercise limits, but you will be responsible for ensuring you do not overdo any activities at home.
At My Health Team we also highly recommend maintaining the rest of your body’s fitness with regular exercise while recovering from surgery. Several types of cardiovascular machines can be used including an upper body bike, a stationary bike, or a treadmill for walking. Cardiovascular activity in a pool may also be appropriate. Your physiotherapist at My Health Team can discuss which cardiovascular activity would be best for you and provide a program for you to maintain your general fitness while you recover from your surgery.
As therapy sessions taper down, your therapist at My Health Team will help you with decisions about getting back to work and your previous recreational activities. Ideally, patients are able to go back to their prior activities, however, some patients may need to modify their activities to avoid future problems.
Generally rehabilitation after surgery for cervical spinal stenosis proceeds very smoothly with the physiotherapy we provide at My Health Team. If for some reason, however, your pain continues longer than it should or therapy is not progressing as your physiotherapist would expect, we will ask you to follow-up with your surgeon to confirm that your neck is tolerating the rehabilitation well and to ensure that there are no complications that may be impeding your recovery.
Portions of this document copyright MMG, LLC.
My Health Team provides services for physiotherapy in Redcliffe.
 Get Immediate Access To Your Special Report And Top Tips From Our PTs!
Get Immediate Access To Your Special Report And Top Tips From Our PTs!


