Introduction
Physiotherapy in Redcliffe for Pediatrics
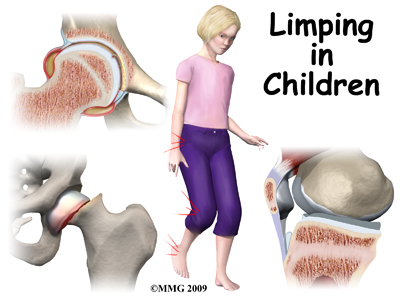
Welcome to My Health Team’s resource about childhood limping.
Limping in a child is a concern. Limping in a child is never normal. It can be caused by many things, sometimes by something minor, like a blister or cut. The most common cause of a limp in young children is a fracture. Sometimes it is caused by a serious infection. Although rare, it can also be caused by a tumor.
This guide will help you understand:
- what can cause this condition
- what the symptoms are
- how your health care professional will diagnose the condition
- what treatment options are available
- what My Health Team’s approach to rehabilitation is
#testimonialslist|kind:all|display:slider|orderby:type|filter_utags_names:Pediatrics|limit:15|heading:Hear from some of our *Pediatrics* patients#
Anatomy
What parts of the body can be involved?
Reasons for limping can involve many parts of the body. The hip, knee, shin bone, ankle, and foot are common parts that can cause limping. Limping can also be caused by problems in the back or pelvis.
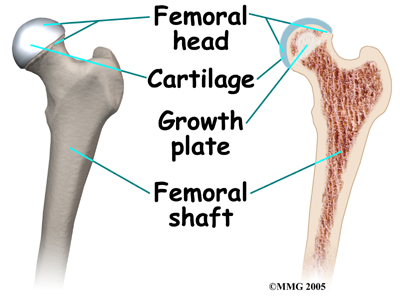
The hip is a ball-and-socket joint. A tough lining called the synovium covers it. The ball of the joint is the end of the thigh bone, called the femur. Like other ends of bones in children, the ball has an area called a growth plate. A growth plate has cells that produce new bone. The growth plate is weaker than other parts of the bone. This makes this area more likely to fracture.
The socket part of the hip joint is called the acetabulum. It is actually part of the pelvis. The acetabulum forms a cup where the ball of the femur sits. It is covered with articular cartilage. Articular cartilage is the material that covers the ends of the bone of any joint. It's a rubbery, slippery substance that allows the surfaces to slide against one another without damage to either surface.
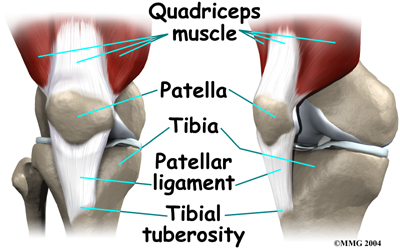
The knee joint is made up of the other end of the femur and the end of the shin bone. The knee cap, or patella, is also part of the knee joint.
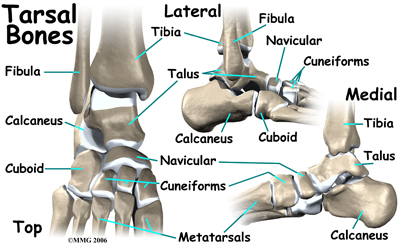
The lower leg is made up of two main bones. The larger bone is the shin bone, called the tibia. The smaller bone runs along the outside of the tibia it's called the fibula. These bones, along with a saddle shaped bone at the top of the foot called the talus form the ankle.
The foot has many bones. There are seven short bones below the ankle called the tarsals. The big square bone on the outside of the middle of the foot is called the cuboid. The long bones of the foot from the arch to the joints of the toes are called the metatarsals.
Tarsals
Causes
What are some common causes of pain that can cause a limp in children?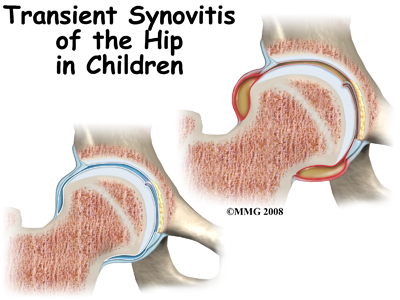 The most common cause of a limp in small children is a fracture. Toddler’s fractures involve buckling or bowing of the tibia (shin bone). This usually happens when a child trips or falls up stairs.
The most common cause of a limp in small children is a fracture. Toddler’s fractures involve buckling or bowing of the tibia (shin bone). This usually happens when a child trips or falls up stairs.
Bunk-bed fractures are caused by jumping. The cuboid bone and first metatarsal in the foot are the bones that are usually broken in this type of injury.
In children from two to ten years old, the most common cause of hip pain is transient synovitis (TS). This involves swelling or inflammation of the synovium of the hip. The synovium is a tough covering of the joint. Often, the child will have had a cold or viral infection just before the hip pain started. Transient synovitis usually lasts ten days. It generally gets better with minimal treatment.
Joint infection of the hip causes a more sudden onset of pain. Children will usually not walk at all when the joint is infected.
Osteomyelitis is an infection of the bone. It usually happens near the ends of the bones, close to the growth plate.
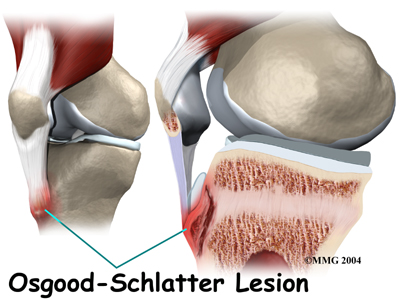
Overuse syndromes are common in active adolescents. Stress fractures of the foot, patellofemoral joint problems, and Osgood-Schlatter's disease are examples of overuse syndromes.
Osgood-Schlatter's Disease
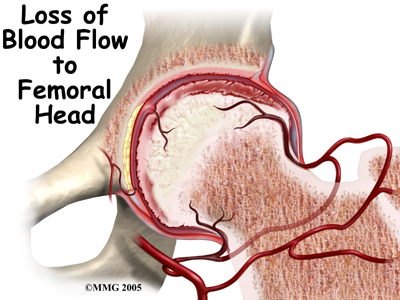
Legg-Calvé-Perthes disease typically affects boys between the ages of five and ten. It is also called osteonecrosis and avascular necrosis of the hip. It literally means death of bone. The ball of the hip dies because the blood supply has been cut off. When this happens, the femoral head and acetabulum will change their shapes over one to three years. The ball of the femur will flatten out. This problem with the hip is often missed at first. It is frequently misdiagnosed as synovitis of the hip.
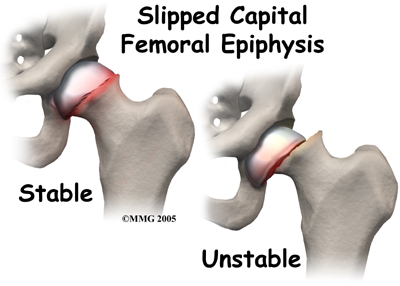
Slipped Capital Femoral Epiphysis
is the slipping of the growth plate of the ball of the hip joint. It usually happens in obese, older children.
Related Document: A Patient's Guide to Slipped Capital Femoral Epiphysis
Tumors in bone are rare in children however they can occur. Ewing’s sarcoma is a cancerous tumor that starts in the bone. More often, a tumor found in the bone is from cancer somewhere else in the body. Neuroblastoma and leukemia are both known to cause destruction of bones.
Rheumatoid arthritis is an auto-immune disease. It can affect children. When it does it is called juvenile onset rheumatoid arthritis. When left untreated it can destroy the synovium of joints, causing deformity, pain, and loss of mobility.
Neuromuscular disease such as muscular dystrophy or other genetic problems may also cause limping.
Back problems, appendicitis, or other problems in the abdomen or pelvis can cause limping, usually in older children.
Symptoms
In addition to limping due to pain, or not walking at all, other symptoms may occur.
Swelling or redness near a joint often means infection or inflammation. Fever or chills can also mean infection. Tenderness of a specific area could be suspicious for a fracture.
As mentioned above, transient synovitis often happens after having a cold or viral infection.
Diagnosis
How does a health care professional diagnose the condition?
Making a diagnosis can be difficult. At My Health Team your physiotherapist will initially take a thorough history of when and how the limping started. It is important to determine if there has been an accident or fall and also important to discern whether or not the limping started suddenly or gradually. Repetitive or strenuous activity may also initiate an injury that causes limping so we may inquire about your child’s activity level. We may also ask you about any other related symptoms such as swelling and redness, or may inquire about whether your child has had a recent illness or cold. Your physiotherapist may ask to watch your child walk to assess the limp during the gait cycle. In addition your physiotherapist will observe your child in standing and possibly sitting or lying to look for any bone alignment problems that may be contributing to their limp.
Next your physiotherapist will then palpate around any areas of pain. As referred pain can cause symptoms in unrelated areas to the actual problem, they may also palpate areas that are not notably painful such as the low back or anywhere along the lower limb. Commonly, for example, problems in the hip will cause symptoms in the knee of a child therefore thorough examination is necessary.
Following palpation your physiotherapist will assess the range of motion of your child’s joints and compare them to the other side. They will also check the strength of the muscles on both sides and may check for the integrity of the ligaments around the joints.
If it is clearly determined from the history and physical examination that your child’s limping is the result of an orthopaedic origin that can be treated by physiotherapy, your physiotherapist will explain the cause of the limp and then discuss the treatment options. If, however, a definitive origin of the pain cannot be determined your physiotherapist will recommend that your child is reviewed by a doctor for further examination and investigative tests to more clearly discern the cause of the limp.
My Health Team provides services for physiotherapy in Redcliffe.
Physician’s Review
Your child’s doctor will also take a thorough history and will want to look at your child’s skin and joints. He/She is looking for things such as cuts, blisters, rash, insect bites, joint swelling and deformity of bones which can be gateways to infections into the joints.
In many cases, laboratory testing and imaging tests (x-rays) are needed to make the right diagnosis.
Since fractures are the most common cause of limping in children, x-rays are done in most cases. In young children, x-rays of the pelvis, hips, and lower legs are recommended.
Magnetic resonance imaging (MRI) allows your doctor to look at slices of the area in question. The MRI machine uses magnetic waves, not x-rays, to show the soft tissues of the body. It is best at evaluating soft-tissue injury and tumors. The test may require the use of dye in an IV. Children may need to have sedation or anesthesia in order to lie still for the test.
Computed tomography (CT) scan may be ordered. It is best for evaluating problems with bones. It is usually tolerated by children; however, it exposes them to radiation.
Bone scans, also called nuclear scans can be used to detect fractures, osteomyelitis, and Legg-Calvé-Perthes disease. A radioactive tracer, Technetium, is injected into your child’s vein. Where there is an increase in metabolic activity, such as in the case with inflammation, fracture, infection, or tumor, the Technetium will be more concentrated.
Ultrasound is another form of imaging that may be used. It uses sound waves to create a picture. Ultrasound of the hip can show osteomyelitis, septic arthritis, transient synovitis, and Legg-Calvé-Perthes disease.
Laboratory studies may also help your child’s doctor make a diagnosis. Most common is a complete blood count (CBC). This checks the white blood cell count which can increase during an infection. When inflammation and infection are present, your erythrocyte sedimentation rate (ESR) and C-reactive protein increase so these lab tests may also be done. Other lab tests may be done, such as rheumatoid factor, sickle cell tests, and lyme disease tests.
If joint or bone infection is suspected, blood cultures can be helpful. Your child’s doctor will likely want the joint aspirated. The bone may need to have a biopsy. A needle is placed in the joint or bone, and some of the fluid is removed and tested. In the case of infection, the bacteria causing the infection can be determined and an appropriate antibiotic treatment can then be chosen.
Your child’s doctor will want to follow up periodically. Sometimes this requires repeat blood work and/or imaging studies.
Treatment
What treatment options are available?
Nonsurgical Treatment
Transient synovitis usually responds to anti-inflammatory medication and rest. Symptoms generally improve after 10 days, with an eventual return to activity.
In the case of infection, six weeks of intravenous (IV) antibiotics is usually required. Sometimes antibiotics taken by mouth can be effective instead of such a long period of IV antibiotics. Your child may need to be in the hospital for a few days at first. Sometimes surgery is necessary to drain the area that is infected.
Referral to a doctor who specializes in arthritis will be necessary if your child is diagnosed with rheumatoid arthritis.
Although tumors are rare in children, they do occur. Some tumors may respond to chemotherapy or radiation. Sometimes the tumor has to be surgically removed.
In toddler’s fractures and bunk-bed fractures, sometimes casts must be used. Limiting weight bearing when walking may mean your child will have to use crutches, or be in a wheelchair for awhile. Your physiotherapist will teach your child how to properly walk with crutches and how to safely manage them on stairs.
Stress fractures and Osgood-Schlatter’s usually respond well to a discontinuation of the activity that caused them while continuing exercises like swimming and stationary biking to maintain conditioning. Your physiotherapist can provide advice on how to best maintain fitness and can design an individualized program for your child to follow while their injury heals.
Patellofemoral joint problems and overuse syndromes usually respond well to physiotherapy treatment. Physiotherapy may even be recommended when the cause of the limp has been determined to be infectious or other in nature (once the initial problem has been cleared up) as limping, even for short periods, can cause your child to lose strength or range of motion in their limb. Your physiotherapist can address these problems to ensure they do not have lasting effects.
In general, most of the causes of limping can be treated without surgery. The majority of children respond well to therapy and resume walking normally without any long-term problems.
My Health Team provides services for physiotherapy in Redcliffe.
Nonsurgical Rehabilitation
Once the cause of your child’s limping has been clearly determined through examination and investigations, your physiotherapist will determine if physiotherapy treatment is required and if so, will decide on the best therapy for your child.
Initially your My Health Team’s physiotherapist may use modalities such as heat, ice, ultrasound, or electrical current to assist with decreasing any pain associated with the cause of the limp. If necessary we may also suggest the use of a brace or use taping to assist with the pain. Your physiotherapist will address your child’s walking pattern and assist your child in gait retraining to ensure they are walking as normal as possible as the problem resolves. If your child continues to find it difficult to walk without limping, your physiotherapist will suggest the use of one or two crutches to normalize their gait and prevent compensatory problems in other areas of the body.
The next part of our treatment will focus on normalizing any deficits that may have developed in the range of motion and strength of the lower limb joints. Your physiotherapist may assist in stretching your child’s limb or lower back while in the clinic and, if necessary, will ‘mobilize’ the joints of your child. This hands-on technique encourages the stiff joints to move gradually into their normal range of motion. In addition to the hands-on treatment in the clinic we will also prescribe a series of stretching exercises that we will encourage your child to do as part of a home exercise program. Generally these exercises will be simple activities that you can incorporate into the everyday activities of your child. For example, if your child is young, your physiotherapist may show you some stretching positions that you can encourage your child to sit or lie in while they play to improve range of motion. If your child is of an adolescent age, formal stretches will be taught and encouraged throughout the day.
Similarly to the range of motion deficits, strength deficits will also be addressed. Again, for young children, your physiotherapist will show you how to incorporate strengthening exercises into your child’s normal activities such as walking or stair climbing, whereas older children will be prescribed a more traditional strength building set of exercises. For all children we may incorporate items such as Theraband into the exercises to provide additional resistance for the limb.
The final part of our My Health Team treatment will be ensuring that your child’s coordination and balance have returned to normal after their injury. Again, after even a short period of not walking or walking with a limp, your child’s normal balance, coordination, and proprioception (the ability to know where your body is without looking at it) can decline in function. Exercises, which may include balancing on one foot, jumping, and quick agility movements, will be encouraged.
Fortunately, gaining lost range of motion, strength, and coordination due to limping goes quickly once the initial cause of the limping has been addressed. You will notice improvements in your child’s function and gait even after just a few treatments with your physiotherapist.
My Health Team provides services for physiotherapy in Redcliffe.
Surgical Treatment
Surgical treatment is specific to the cause of the problem.
In the case of slipped capital femoral epiphysis, surgery is often required. The femur can be pinned through the skin (percutaneous pinning). The surgeon may need to open the joint to place pins in it. Sometimes the hip that is not affected is also pinned because it is also likely to slip.
Legg-Calve-Perthes often requires surgery to shape the hip joint.
Tumors are rare in children but they do occur. Your child will probably be referred to a specialist to determine the best method of treatment for the type of tumor discovered. Some tumors respond to chemotherapy or radiation. Surgical excision (removal) may be necessary.
Osteomyelitis sometimes requires a surgeon to open the area. This allows drainage of the infectious fluid and removal of damaged tissue and bone if needed.
Post Surgical Rehabilitation
Rehabilitation post-surgically can begin once your child’s surgeon indicates that it is safe to do so. Each particular type of surgical procedure performed will have rehabilitation guidelines specific to that surgery. Your physiotherapist at My Health Team will liaise with your surgeon regarding the specific restrictions that he or she requires for your child and will discuss with you what to expect during your child’s individual rehabilitation process.
The goals of physiotherapy post-surgically are similar to the goals of physiotherapy discussed above under nonsurgical rehabilitation. Thus, once your child’s surgeon indicates that physiotherapy can begin, your physiotherapist will work to reduce associated pain, retrain your child’s gait, and address any deficits in range of motion, strength, coordination, balance, and proprioception.
If your child’s pain continues longer than it should or physiotherapy is not progressing as your physiotherapist would expect, we will ask you to follow-up with your child’s surgeon to confirm that there are no post-surgical complications that may be impeding your child’s recovery. Generally, however, children who have required surgery to correct the problem causing their limp respond very well to the post-surgical physiotherapy we provide at My Health Team. Under the supervision of one of our physiotherapists your child should be back to the daily activities they enjoy in no time.
My Health Team provides services for physiotherapy in Redcliffe.
 Get Immediate Access To Your Special Report And Top Tips From Our PTs!
Get Immediate Access To Your Special Report And Top Tips From Our PTs!